
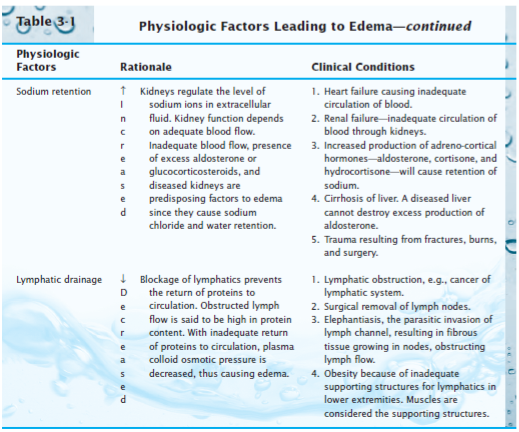
Lymphedema represents a third form and may result from impaired lymph pump activity, an increase in lymphatic permeability favoring protein flux from lumen to interstitial fluid, lymphatic obstruction (e.g., microfiliarisis), or surgical removal of lymph nodes, as occurs in the treatment of breast cancer. Hydrostatic edema refers to accumulation of excess interstitial fluid which results from elevated capillary hydrostatic pressure while permeability edema results from disruption of the physical structure of the pores in the microvascular membrane such that the barrier is less able to restrict the movement of macromolecules from the blood to interstitium. Ascites can predispose afflicted individuals to peritoneal infections, hepatic hydrothorax, and abdominal wall hernias. Ascites, or the pathologic accumulation of fluid in the peritoneal cavity, occurs in cirrhosis and is caused by fluid weeping from congested hepatic sinusoids secondary to elevated portal venous pressure.
Filtration-secretion may compromise the absorptive function of the delicate intestinal mucosa and appears to occur as a result of the formation of large channels between mucosal cells in the villous tips when interstitial fluid pressure increases by greater than 5 mmHg. In the intestine, unrestrained transcapillary filtration leads to exudation of interstitial fluid into the gut lumen, a phenomenon referred to as filtration-secretion or secretory filtration. This, in turn, reduces the vascular transmural pressure gradient and physically compresses capillaries, thereby reducing nutritive tissue perfusion. As a consequence of the inability of these tissues to readily expand their interstitial volume, relatively small increments in transcapillary fluid filtration induce large increases in interstitial fluid pressure. For example, the kidneys are enveloped by a tough fibrous capsule, the brain is surrounded by the cranial vault, and skeletal muscles in the volar and anterior tibial compartments are encased in tight fascial sheaths.

In some tissues, certain anatomical structures limit the expansion of the tissue spaces in response to edemagenic stress. These are especially important problems in the lungs, where pulmonary edema can significantly impair gas exchange. For the same reason, edema formation also limits the diffusional removal of potentially toxic byproducts of cellular metabolism. Our focus is on swelling of the extracellular matrix or interstitial edema, which may occur as a result of aberrant changes in the pressures (hydrostatic and oncotic) acting across the microvascular walls, alterations in the molecular structures that comprise the barrier to fluid and solute flux in the endothelial wall that are manifest as changes in hydraulic conductivity and the osmotic reflection coefficient for plasma proteins, or alterations in the lymphatic outflow system, as predicted by examination of the Starling equation.Įxcessive accumulation of interstitial fluid is generally viewed as detrimental to tissue function because edema formation increases the diffusion distance for oxygen and other nutrients, which may compromise cellular metabolism in the swollen tissue. Edema occurs when an excessive volume of fluid accumulates in the tissues, either within cells (cellular edema) or within the collagen-mucopolysaccharide matrix distributed in the interstitial spaces (interstitial edema).


 0 kommentar(er)
0 kommentar(er)
